With the ongoing debate around prospective access to patient records, we have looked at an improved offer for our local patients across the North East London ICS region. This is as an alternative to the automatic prospective access that NHSE have proposed and are asking practices to sign up to.
We are encouraging all our patients to interact with NHS services through the NHS App as this will also allow patients to:
– Request repeat prescriptions
– Access their medical record (prospectively and retrospectively)
– Consult with their GP practice via the practice online consultation tool
– Review secondary care appointments
– View their care planning documentation (via PKB)
It is also important for practices to be aware that:
- Sensitive information may be hidden from the patient’s view. This can either be done when the consultation is written up, or later when reviewing the notes. Details for EMIS Web here
- Access to the medical record can be enabled for documents and consultations from a certain date. This makes it much safer in respect of inappropriate access to, say third party information.
With the current NHSE request to enable all patients for prospective access automatically prospectively there is no oversight of who gets access eg on any patients who may be coerced, have safeguarding issues or those that may have their records accessible by another family member. Even if the pilot tool was run to exclude patients with sensitive codes, this may not capture all the necessary patients. Having an opting in process allows the practice to remain in control and also allow patient records to be reviewed on a iterative basis providing more access for patients. As an example of workload that is generated from opening up access, I’ve done a mini audit at our practice and the access to records is generating 2-3 queries a week from patients questioning something that they have seen on their online record – this is additional workload that we could have control over – if automatic access was granted then this workload uncontrollably increases by stealth. And then there’s the issue of who is the actual data controller of the record……. which NHSE have not provided any clarity on.
There are benefits to patients for allowing access to the medical record and these include:
- Patients have access to their problem list as well as medications that they can share freely to help manage their health. This is particularly beneficial for patients who have long term conditions
- When blood tests or investigations are requested, patients can obtain the result, along with a comment from their GP, without having to contact the GP practice
- Document access will allow patients to share in the letters sent to and from the hospital
- Allowing access to the medical record will help reduce access for Subject Access Requests under GDPR
- Access to immunisations will enable patients to know what they have had previously
- One study showed that if 30% of your patients have FULL record access and use it at least twice a year, a practice is likely to save 10% of appointments and 100s of telephone calls. Link to reference.
There are global settings that need to be configured at an organisational level and these can then be further adjusted for each individual patient as required. This includes, for example, switching on GP comments for test results.
These recommendations apply to patients over the age of 16. Under 16s can also be granted personal access if they are deemed to be Gillick competent by their clinician. If a patient under the age of 16 is given their own access, it is recommended that a code is applied to the patients medical records such as:
EMISNQCO278 (Competent to consent to online access)
Online Access
When hovering over the icon in the patient precis bar, you can see the online status of the active patient

The colour of the icon signifies:
Green = Live (fully registered)
Amber = Inactive or Active (not activated access)
Black = Not registered
Proxy Access
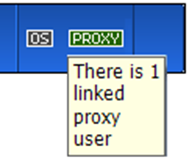
Proxy access has also been developed further and further details are available on this from system suppliers. The details for EMIS are available here.
To note – patients with proxies allocated will be identified in the patient precis bar.
For children, proxy access is restricted at age 11 (to book one appointment) and then revoked at age 16.
Recommended Approach for GP Practices within North East London (NEL) CCG
Practice Processes
Practices should be able to register a test patient for online accesses and to ensure that all practice staff are aware of how the services are available and shown to patients online. This could be done within a practice staff meeting for example.
Staff should also be encouraged to register for online access at their own GP practices and to share learning of what they feel works well and what could be improved as a way to improve patient experience.
Once logged in with a test patients as a minimum the following should be reviewed:
– View medications
– See how repeat prescriptions are ordered
– Review which appointments are being shown – and how they are displayed
– Which investigations are viewable
– Are consultations viewable – and how back they are viewable.
This may, for example, lead to the practice reviewing how they want to configure their appointment offering for patients. There is also the option of configuring the clinical system for messages to be displayed informing the patients of practice processes for medication requests or booking appointments.
Practices may want to restrict the access of consultations, free text etc to only be viewed from a certain date in time so that they are confident that robust processes are in place for good information governance within the practice. This can be configured from the online access global settings. The NHSE guidance is to set this from 1/1/1900 but practices should set a date that they are comfortable with if they feel that this is not appropriate. Guidance for EMIS Web here.
Practices should also consider how they consent their patients for online access to their medical record and if they wish their patients to consider some important points such as ensuring that patients will keep their information safe and secure, understanding that they may see abnormal results, ensuring that they are not coerced etc.
Practices are strongly advised to consent patients ideally through a custom Florey that is available to all NEL GP practices:
– click this link to obtain the Florey Questionnaire for Patient Online Access
To increase patient uptake, the process to obtain online codes for detailed medical record access should be made simpler for patients as well as reduce administrative burden for practices.
A common administrative burden that practices have is that they do not release access until notes are reviewed in case something needs to be redacted or withheld. In the vast majority of cases, access is granted to patients without any redaction.
To improve the process one suggestion is that patients are given access at the point of request and verification and a clinical review of the notes occurs later, thereby reducing the number of steps in the process.
Suggested Practice Processes
- Ensure that practices have set EMAS manager to a particular date from which retrospective medical record access is available to all patients (default is 1/1/1900 for all records) – ONE OFF PROCESS
- The AccuRx Florey is set up at the practice (see above) – ONE OFF PROCESS
- Have a clear pathway for patients to request access to their medical records through the NHS App that both patients and staff understand. Promotion of the NHS App is encouraged to be advertised via the practice website.
- The patient process as below is clear to all practice staff dealing with patient requests.
Suggested Patient Processes
- Patient requests online access
- Practice issues patient with access information via AccuRx Florey
- Patient completes and returns Florey that is saved in the patients notes
- Practice will further verify the identity of the patient if required
- A code “314191000000103” (Patient registration data verified) should be added to the medical record
- Patients are either:
- – given full prospective access as per the request on their application form at the point of verification (the practice would need to then review and allow retrospective access within a set time period (eg 2 weeks)
- – informed that their request will be processed within a set time period (eg 2 weeks)
- The practice will then review the records within a set time period (aiming for 2 weeks) and it is recommended that this is also an opportunity for clinicians to tidy up the medical record to ensure:
- – The problem list is accurate with significant, active and minor problems accurately coded
- – Medications are appropriate and repeat medications are correctly listed and linked
- – Any data deemed confidential is marked as such